Our Health Library information does not replace the advice of a doctor. Please be advised that this information is made available to assist our patients to learn more about their health. Our providers may not see and/or treat all topics found herein.
Carotid Endarterectomy
Surgery Overview
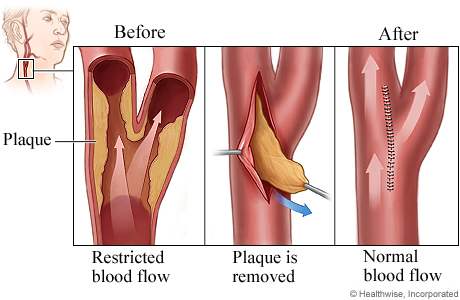
A carotid endarterectomy (say "kuh-RAW-tid en-dar-tuh-REK-tuh-mee") is done to remove fatty buildup (plaque) from one of the carotid arteries. There are two of these arteries. One runs along each side of the neck. They supply blood to your brain. When plaque builds up in either one, it can limit blood flow to your brain. The plaque also raises your risk of stroke. This surgery may lower your risk of stroke.
The doctor will make a cut (incision) in your neck. Then the doctor will make a cut in the carotid artery and take out the plaque.
Next, the doctor will close the cut in the artery with stitches. The doctor may sew a man-made or tissue patch to close the cut in the artery. Then the doctor will use stitches to close the cut in your skin. It will leave a scar. But the scar will fade with time.
You may stay in the hospital for at least 1 or 2 days.
How It Is Done
During carotid endarterectomy, your surgeon:
- Makes a cut in your neck just below the jaw.
- Opens the carotid artery and carefully removes the plaque.
- May sew (graft) a man-made or tissue patch onto the carotid artery to help close the cut.
- Closes the artery and skin incisions with stitches.
What To Expect
You may stay in the hospital for at least a day or two.
You may have a sore throat for a few days. You can expect the incision to be sore for about a week. The area around it may also be swollen and bruised at first. The area in front of the incision may be numb. This numbness usually gets better after several months.
You may feel more tired than usual for several weeks after surgery. You can do light activities around the house. But don't do anything strenuous until your doctor says it is okay. This may be for at least 2 weeks.
You will have regular tests to check blood flow in your carotid arteries.
Why It Is Done
Carotid endarterectomy is done to help lower your risk of stroke.
Your doctor may recommend this procedure based on certain things. These include:footnote 1, footnote 2, footnote 3
- The amount of narrowing (stenosis) in your carotid arteries. A procedure may be an option if the narrowing is 50% or more.
- Whether you had a stroke or TIA within the past 6 months. If you have not had a stroke or TIA, it's less clear that the procedure will help you.
Your doctor can help you understand your risk of stroke and whether endarterectomy might be an option for you.
Learn more
How Well It Works
If you have not had a TIA or stroke
For people who haven't had a stroke or TIA, it's not clear when endarterectomy might be a good choice. The surgery may help prevent a stroke in the long run. But in the short term, it increases the risk of stroke and death. Medicine and a heart-healthy lifestyle may work as well as surgery to prevent a stroke. And they don't have the risks of surgery.
It's not clear that this surgery will reduce your stroke risk more than medicines and lifestyle changes alone.footnote 4, footnote 5 Studies are being done to compare current medical therapy with endarterectomy.
If you've had a TIA or stroke
An endarterectomy can help lower your risk of stroke if your carotid artery is narrowed by 50% or more. People with less than 50% narrowing do not benefit from surgery.footnote 6, footnote 7
You may benefit most from endarterectomy if it is done within 2 weeks of the stroke or TIA.footnote 6, footnote 7
Risks
The risks of carotid endarterectomy include:
- Infection.
- Nerve damage that could cause serious problems, like trouble swallowing.
- Bleeding in the brain or neck.
- Stroke, heart attack, or death.
- The artery can narrow again.
The risks of a procedure depend on things like your age and your overall health. Who does the procedure and where it is done are also important.
References
Citations
- Meschia JF, et al. (2014). Guidelines for the primary prevention of stroke: A statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke, published online October 28, 2014. DOI: 10.1161/STR.0000000000000046. Accessed October 29, 2014.
- Kleindorfer DO, et al. (2021). 2021 Guideline for the prevention of stroke in patients with stroke and transient ischemic attack: A guideline from the American Heart Association/American Stroke Association. Stroke, 52(7): e364–e467. DOI: 10.1161/STR.0000000000000375. Accessed June 4, 2021.
- AbuRahma AF, et al. (2021). Society for Vascular Surgery clinical practice guidelines for management of extracranial cerebrovascular disease. Journal of Vascular Surgery, published online June 19, 2021. DOI: 10.1016/j.jvs.2021.04.073. Accessed July 19, 2021.
- Meschia JF, et al. (2014). Guidelines for the primary prevention of stroke: A statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke, published online October 28, 2014. DOI: 10.1161/STR.0000000000000046. Accessed October 29, 2014.
- AbuRahma AF, et al. (2021). Society for Vascular Surgery implementation document for management of extracranial cerebrovascular disease. Journal of Vascular Surgery, published online June 19, 2021. DOI: 110.1016/j.jvs.2021.04.074. Accessed July 20, 2021.
- Kleindorfer DO, et al. (2021). 2021 Guideline for the prevention of stroke in patients with stroke and transient ischemic attack: A guideline from the American Heart Association/American Stroke Association. Stroke, 52(7): e364–e467. DOI: 10.1161/STR.0000000000000375. Accessed June 4, 2021.
- AbuRahma AF, et al. (2021). Society for Vascular Surgery clinical practice guidelines for management of extracranial cerebrovascular disease. Journal of Vascular Surgery, published online June 19, 2021. DOI: 10.1016/j.jvs.2021.04.073. Accessed July 19, 2021.
Credits
Current as of: October 2, 2025
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Ignite Healthwise, LLC education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
Current as of: October 2, 2025
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Ignite Healthwise, LLC education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
This information does not replace the advice of a doctor. Ignite Healthwise, LLC disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use and Privacy Policy. Learn how we develop our content.
To learn more about Ignite Healthwise, LLC, visit webmdignite.com.
© 2024-2025 Ignite Healthwise, LLC.


